RS Sentolo Dilengkapi Autis Center
 SENTOLO – Pemkab Kulonprogo menargetkan Rumah Sakit Tipe D bisa beroperasi awal 2014. Pembangunan dilakukan menggunakan tanah kas desa di Desa Banguncipto, Sentolo.Bupati Kulonprogo Hasto Wardoyo mengatakan pembangunan RS Sentolo terus berjalan. Saat ini proses pembebasan lahan, sedangkan pembangunan fisik ditargetkan selesai Desember 2013.“Kemudian awal Januari 2014 mulai beroperasi meski belum sempurna,” kata Hasto, kemarin (29/4).Hasto menjelaskan, pembangunan tahap pertama menggunakan lahan 6.500 meter persegi. Pemkab juga berencana membangun Autis Center dengan lahan 6.000 meter persegi.“Nanti izin gubernur dengan kompensasi. Kami tidak menggunakan tanah warga karena tanah kas desa sudah mencukupi,” kata Hasto.RS tersebut mengantisipasi banyaknya pasien di RSUD Wates yang tidak dapat ditampung karena tempat tidur terbatas. Akan dilengkapi 100 tempat tidur dan diarahkan sebagai RS tanpa kelas.Hal ini untuk mengantisipasi pelaksanaan aturan Badan Penyelenggara Jaminan Sosial (BPJS). Sistemnya, setiap pasien yang dirawat mendapatkan layanan kelas I namun dengan biaya perawatan sama seperti harga kelas III.“Dengan aturan ini semua pasien diperlakukan sama oleh tenaga medis, tidak ada yang diprioritaskan,” kata Hasto.Bupati Hasto mengatakan RS tersebut akan dikembangkan menjadi pusat pengobatan kanker. Karena pelayanan kanker di DIJ tidak cukup memadahi, diharapkan mampu melayani pasien dari DIJ maupun Jateng.“Tenaga medis akan dioptimalkan dari RS dan puskesmas di Kulonprogo,” katanya.Kepala Badan Perencanaan Pembangunan daerah (Bappeda) Kulonprogo Agus Langgeng Basuki mengatakan, anggaran tahap pertama Rp 6 miliar dari APBD Kulonprogo. Sedangkan, anggaran yang dibutuhkan Rp 20 miliar dari APBD Provinsi.“Pembangunan secara bertahap. Kementerian Kesehatan juga akan memberi bantuan Rp 10 miliar dalam bentuk perawatan medis untuk mendukung beroperasinya RS tersebut,” kata Agus. (asa/iwa)
SENTOLO – Pemkab Kulonprogo menargetkan Rumah Sakit Tipe D bisa beroperasi awal 2014. Pembangunan dilakukan menggunakan tanah kas desa di Desa Banguncipto, Sentolo.Bupati Kulonprogo Hasto Wardoyo mengatakan pembangunan RS Sentolo terus berjalan. Saat ini proses pembebasan lahan, sedangkan pembangunan fisik ditargetkan selesai Desember 2013.“Kemudian awal Januari 2014 mulai beroperasi meski belum sempurna,” kata Hasto, kemarin (29/4).Hasto menjelaskan, pembangunan tahap pertama menggunakan lahan 6.500 meter persegi. Pemkab juga berencana membangun Autis Center dengan lahan 6.000 meter persegi.“Nanti izin gubernur dengan kompensasi. Kami tidak menggunakan tanah warga karena tanah kas desa sudah mencukupi,” kata Hasto.RS tersebut mengantisipasi banyaknya pasien di RSUD Wates yang tidak dapat ditampung karena tempat tidur terbatas. Akan dilengkapi 100 tempat tidur dan diarahkan sebagai RS tanpa kelas.Hal ini untuk mengantisipasi pelaksanaan aturan Badan Penyelenggara Jaminan Sosial (BPJS). Sistemnya, setiap pasien yang dirawat mendapatkan layanan kelas I namun dengan biaya perawatan sama seperti harga kelas III.“Dengan aturan ini semua pasien diperlakukan sama oleh tenaga medis, tidak ada yang diprioritaskan,” kata Hasto.Bupati Hasto mengatakan RS tersebut akan dikembangkan menjadi pusat pengobatan kanker. Karena pelayanan kanker di DIJ tidak cukup memadahi, diharapkan mampu melayani pasien dari DIJ maupun Jateng.“Tenaga medis akan dioptimalkan dari RS dan puskesmas di Kulonprogo,” katanya.Kepala Badan Perencanaan Pembangunan daerah (Bappeda) Kulonprogo Agus Langgeng Basuki mengatakan, anggaran tahap pertama Rp 6 miliar dari APBD Kulonprogo. Sedangkan, anggaran yang dibutuhkan Rp 20 miliar dari APBD Provinsi.“Pembangunan secara bertahap. Kementerian Kesehatan juga akan memberi bantuan Rp 10 miliar dalam bentuk perawatan medis untuk mendukung beroperasinya RS tersebut,” kata Agus. (asa/iwa)
Sumber: http://www.radarjogja.co.id
Australian Nursing Federation Welcomes Improved Security at Dandenong Hospital
 Earlier today, the hospital announced it would bring in a strategy for dealing with violent patients after nurses threatened to strike following weeks of escalating emergency room violence.
Earlier today, the hospital announced it would bring in a strategy for dealing with violent patients after nurses threatened to strike following weeks of escalating emergency room violence.
The most recent attack was on Sunday when a man threw pieces of concrete at the waiting room, smashing four windows and terrifying staff and patients.
Monash Health media manager Suzana Talevski said the hospital would implement a protocol mid-year to deal with aggressive and violent patients and visitors, and immediately increase the number of security guards in the department.
ANF Victorian branch assistant secretary Paul Gilbert said it was a very positive response to nurses’ concerns.
“We will be recommending that at this stage they don’t exercise the powers to cease work under the Victorian workplace health and safety laws,” he said.
Dandenong nurses will meet tomorrow afternoon to discuss the new safety measures.
Source: heraldsun.com.au
Half of Terminal Cancer Patients Die in Hospital, Report Says
More than 25,000 people died of cancer in acute-care hospitals in 2011-12
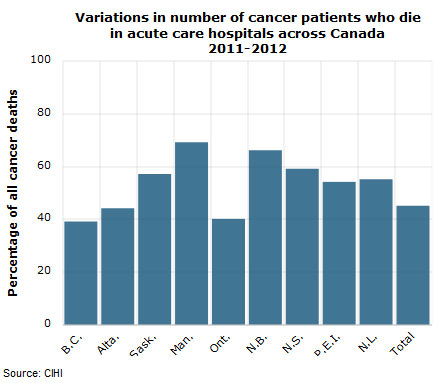
About half of deaths among terminal cancer patients in Canada happen in hospitals, according to a new report.
The Canadian Institute for Health Information looked at end-of-life care for people with cancer across the country, excluding Quebec.
More than 25,000 people — or 45 per cent of all cancer deaths — died in acute-care hospitals in 2011-12, the institute said in its report Tuesday.
“What our study found was a bit of a mismatch between where patients said they wanted to die, which was at home, and where they did spend their last days,” said Kathleen Morris, the group’s director of health system analysis and emerging issues in Toronto.
“Many of the lesson learned from this study extend to anyone at end of life. People are looking for a well co-ordinated system, to have consistent caregivers, to have their pain managed and to be provided with the support they need.”
CIHI said the percentage of cancer patients who die in hospital ranges from 69 per cent in Manitoba to 39 per cent in British Columbia. Differences in the availability and location of palliative care beds in some provinces may be contributing to the variations between provinces in in-hospital beds, the group said.
In Winnipeg, end-of-life patients get dedicated doctors and case workers who oversee care outside of hospitals, said Dr. Michael Hosta of the Winnipeg Regional Health Authority.
“One of the unique aspects to our service is the ability to directly access palliative care beds, bypassing the emergency department,” Hosta said.
Strengthening services outside hospital
About 82 per cent of patients had a documented palliative care diagnosis during their last admission. It’s not known what specific palliative care services people received, or how many may have had access to it at hospices or through home care.
When Teresa Pilarski, 86, died of breast cancer at her daughter’s Toronto-area home on April 12, the family said they wanted to respect the frail woman’s wishes not to treat the cancer and to spend her final days as comfortable as possible in a familiar setting.
Daughter Dorothy Pilarski called the at-home palliative care from myriad professionals an “outstanding” complement to the support of family members and friends.
“She did express a tremendous amount of gratitude and a tremendous amount of affection, and that kept us going,” Dorothy Pilarski said, her voice breaking with emotion.
The experience was so rewarding that the family wants to encourage others to consider the option.
Pilarski’s physician, Dr. Harvey Pasternak, said the goal is to control symptoms with less anxiety to the patient and to their family.
CIHI also reported that 30 per cent of rural residents with cancer had multiple hospital admissions in their last four weeks of life, compared to 20 per cent of the urban residents.
Multiple hospital visits near the end of life can be difficult for individuals and their caregivers, when compared with care received at home, in a nursing home or a hospice, Morris acknowledged.
“Anything that can be done to improve the consistency of care and co-ordination would be very helpful,” she said.
Strengthening services outside the hospital system, such as through family doctors, hospice care or support in the home, are all possibilities, Morris said.
Source: http://www.cbc.ca
Demo Pekerja Juga Usung Isu Kesehatan
 Jakarta, PKMK. Demonstrasi pekerja menyambut Hari Buruh di ibukota, diwarnai dengan sejumlah tuntutan terkait jaminan kesehatan. Hal tersebut terlihat dari spanduk ataupun kostum yang ada di lokasi demonstrasi di sepanjang Jalan Sudirman dan Jalan Thamrin (1/5/2013). Sejumlah pekerja demonstran mengenakan kaus merah bertuliskan “Tolak Upah Murah, Laksanakan BPJS”. Kemudian, di beberapa bus, terpasang spanduk dengan tulisan : “Berlakukan BPJS Kesehatan untuk Seluruh Warga Mulai 1 Januari 2014. Bukan Bertahap”. Selanjutnya, sejumlah pekerja pun mengenakan kaus bertuliskan: “Jamsostum, Jaminan Sosial Tolak Upah Murah”. Beberapa ambulans tampak siaga di sepanjang Jalan Sudirman ataupun Jalan Thamrin. Ambulans milik Partai Demokrasi Indonesia Perjuangan (PDIP) berjumlah kira-kira lima unit. Sedangkan ambulans milik Palang Merah Indonesia berjumlah lima pula. Seorang petugas ambulans PDIP mengatakan, pihaknya belum menemui pekerja demonstran yang sakit serius. “Baru merawat satu demonstran yang sakit biasa. Pusing-pusing,” ujar dia. Sementara, sampai sore ini, aliran demonstran masih mengalir ke arah Monumen Nasional. Situasi terlihat tertib; petugas keamanan dari Kepolisian RI siaga di sepanjang jalan.
Jakarta, PKMK. Demonstrasi pekerja menyambut Hari Buruh di ibukota, diwarnai dengan sejumlah tuntutan terkait jaminan kesehatan. Hal tersebut terlihat dari spanduk ataupun kostum yang ada di lokasi demonstrasi di sepanjang Jalan Sudirman dan Jalan Thamrin (1/5/2013). Sejumlah pekerja demonstran mengenakan kaus merah bertuliskan “Tolak Upah Murah, Laksanakan BPJS”. Kemudian, di beberapa bus, terpasang spanduk dengan tulisan : “Berlakukan BPJS Kesehatan untuk Seluruh Warga Mulai 1 Januari 2014. Bukan Bertahap”. Selanjutnya, sejumlah pekerja pun mengenakan kaus bertuliskan: “Jamsostum, Jaminan Sosial Tolak Upah Murah”. Beberapa ambulans tampak siaga di sepanjang Jalan Sudirman ataupun Jalan Thamrin. Ambulans milik Partai Demokrasi Indonesia Perjuangan (PDIP) berjumlah kira-kira lima unit. Sedangkan ambulans milik Palang Merah Indonesia berjumlah lima pula. Seorang petugas ambulans PDIP mengatakan, pihaknya belum menemui pekerja demonstran yang sakit serius. “Baru merawat satu demonstran yang sakit biasa. Pusing-pusing,” ujar dia. Sementara, sampai sore ini, aliran demonstran masih mengalir ke arah Monumen Nasional. Situasi terlihat tertib; petugas keamanan dari Kepolisian RI siaga di sepanjang jalan.
WNI Jadi Korban Malapraktik Rumah Sakit di Malaysia Usai Operasi Caesar
 TRIBUNNEWS.COM, JAKARTA – Seorang warga negara Indonesia (WNI) yang bekerja Malaysia bernama Rupanlangi Sari Dewi Kalawa diduga menjadi korban malapraktik rumah sakit di Malaysia.
TRIBUNNEWS.COM, JAKARTA – Seorang warga negara Indonesia (WNI) yang bekerja Malaysia bernama Rupanlangi Sari Dewi Kalawa diduga menjadi korban malapraktik rumah sakit di Malaysia.
Sari Dewi yang merupakan karyawan di Mandiri Remittance Malaysia ini masih terbaring di rumahnya di Depok Jawa Barat.
“Kami menduga korban mengalami malapraktik di rumah sakit Malaysia,” ujar Kuasa Hukum Korban, Andreas Sapta Finady, di Jakarta, Senin (29/4/2013).
Sari Dewi kini hanya bisa tergolek di tempat tidur. Perlakuan rumah sakit membuatnya buta, lumpuh, dan tidak bisa berbicara serta tidak bisa bergerak sama sekali setelah sekian lamanya mendapat perawatan.
“Beliau WNI dan bersuamikan warga negara Malaysia,” kata pengacara dari Art and Associated ini.
Nasib naas dialami korban bermula ketika melahirkan anak pertamanya namun oleh pihak rumah sakit diminta melakukan operasi cesar.
Tak dinanya dalam perkembangannya pihak rumah sakit melakukan berbagai operasi pembedahan otak, tengkorak depan kiri atas dibuka.
Ini membuatnya buta, lumpuh, dan tidak bisa berbicara sampai hari ini.
“Kejadiannya dua tahun lalu dan sampai sekarang belum mendapatkan respon dari semua pihak terutama pemerintah. Kami terus mendorong pemerintah untuk memberi perhatian penuh atas masalah ini,” katanya
Kini perempuan cantik yang tak berdaya itu mengundang sejumlah relawan dari dalam negeri untuk memperjuangkan hak-haknya. Para relawan datang dari berbagai kalangan seperti advokat, pemerhati masalah perempuan, dan berbagai unsur lapisan masyarakat lainnya.
“KBRI di Malaysia sudah tahu dan sebenarnya kasus ini kami tindaklanjuti. Ini persoalan kemanusiaan kita dorong pemerintah memberi bantuan. Baik upaya mediasi maupun upaya advokasi.
Kita kedepankan mediasi daripada yuridis formil. Kita sudah surati Kementerian Luar Negeri dan belum menerima respon,” kata dia.
Diduga karena kesalahan prosedur penanganan di rumah sakit itu menyebabkan korban masih terus menderita sakit sampai sekarang dan dapat menyebabkan kematian.
Korban juga sampai hari ini masih terpisah dari anaknya yang dilahirkannya dan berharap suatu ketika bisa bertemu darah dagingnya itu.
“Kami meminta pihak terkait rumah sakit di Malaysia mempertanggungjawabkan masalah ini sampai korban dinyatakan pulih seperti sedia kala,” ujarnya.
Sementara itu Pemerhati Masalah Perempuan, Esther RM Mandalawati, mengatakan masalah ini harus menjadi keprihatinan semua elemen bangsa saat seorang perempuan mendapat perlakuan tidak adil di negeri seberang.
“Ini akan menjadi masalah nasional dan patut untuk diselidiki. Saya minta publik sampaikan ini karena masalah ini tidak main-main,”kata dia.
Pemerintah Indonesia, menurut dia, harus memerhatikan masalah ini serta penjelasan dari pihak rumah sakit di Malaysia harus mengklarifikasi kepada lawyer korban.
“Agar tidak terjadi lagi kasus seperti ini dikemudian hari,” ujar tokoh perempuan asal Indonesia Timur ini.
Dia berterima kasih atas perhatian beberapa relawan yang memerhatikan masalah ini sebab jika hal seperti ini dibiarkan terus-menerus akan menjadi pembiaran terhadap hak-hak kaum perempuan.
“Persoalan ini tidak boleh luput dari seluruh warga. Perlakuan warga negara lain terhadap warga kita,” kata dia.
Sumber: tribunnews.com
Dana Rujukan Rp 1 Miliar Tapi RS Jiwa Belum Berfungsi
 TRIBUNNEWS.COM, KUPANG – Anggota Dewan Perwakilan Rakyat Republik Indonesia (DPR RI) asal daerah pemilihan NTT, Anita Jacoba Gah, meminta Badan Pemeriksa Keuangan (BPK) mengaudit Rumah Sakit Jiwa (RSJ) Naimata. Pasalnya, sudah dialokasikan dana rujukan pasien sekitar Rp 1 miliar, tetapi rumah sakit itu belum berfungsi.
TRIBUNNEWS.COM, KUPANG – Anggota Dewan Perwakilan Rakyat Republik Indonesia (DPR RI) asal daerah pemilihan NTT, Anita Jacoba Gah, meminta Badan Pemeriksa Keuangan (BPK) mengaudit Rumah Sakit Jiwa (RSJ) Naimata. Pasalnya, sudah dialokasikan dana rujukan pasien sekitar Rp 1 miliar, tetapi rumah sakit itu belum berfungsi.
Ditemui Pos Kupang (Tribunnews.com Network) usai bertemu Kepala Dinas Kesehatan Provinsi NTT, dr. Stef Bria Seran, di Kantor Dinas Kesehatan NTT, Sabtu (27/4/2013), Anita mengungkapkan, dana rujukan bagi pasien RSJ Naimata itu bersumber dari APBN tahun 2012.
Anita mengatakan, penjelasan dari Kepala Dinas Kesehatan Provinsi NTT, dr. Stef Bria Seran, bahwa RSJ Naimata belum berfungsi.
“Tapi kok sudah ada alokasi anggaran dari APBN tahun 2012 untuk dana rujukan pasien sakit jiwa. Ini aneh,” kritik Anita.
Terpisah, Kepala Dinas Kesehatan Propinsi NTT, dr. Stef Bria Seran mengatakan, RSJ Naimata belum berfungsi/dimanfaatkan karena pembangunannya belum selesai.
“Sekarang ini dalam proses pembangunan. Kalau sudah selesai dibangun baru bisa digunakan. Untuk rumah sakit jiwa dibutuhkan biaya sekitar Rp 70 miliar, tetapi yang dialokasikan baru Rp 3 miliar,” ungkap Stef.
Stef mengatakan, setiap tahun Dinas Kesehatan NTT mengusulkan dana untuk biaya pembangunan RSJ Naimata itu, tetapi ditolak oleh pemerintah pusat karena anggaran tidak ada.
“Bangunan yang ada sekarang ini sudah dibangun sejak tahun 2007. Sekarang ada dua bangunan yang berdiri di sana,” ujarnya.
Anita juga meminta BPK mengaudit Rumah Sakit (RS) Naibonat, RS Sabu Raijua, dan Rumah Sakit Umum (RSU) Prof. Dr. WZ Johannes Kupang.
“Melalui Komisi IX yang membidangi kesehatan, saya akan minta BPK audit sejumlah rumah sakit tersebut,” katanya.
Ia mengatakan, sekarang ini masa reses anggota DPR RI. “Saya kembali ke Jakarta pada 15 Mei 2013. Sampai di sana, melalui komisi IX saya minta BPK audit rumah sakit empat rumah sakit itu,” ujar Anita.
Sumber: tribunnews.com
Hospital beds in Shipston cut as care is given at home
 South Warwickshire NHS Foundation Trust said there were many benefits for patients receiving care at home, including building patient confidence in their own environment, reducing the risk of falls and losing muscle strength, less risk of catching infections, enabl-ing tailored care plans, as well as easing the transition from hospital back home.
South Warwickshire NHS Foundation Trust said there were many benefits for patients receiving care at home, including building patient confidence in their own environment, reducing the risk of falls and losing muscle strength, less risk of catching infections, enabl-ing tailored care plans, as well as easing the transition from hospital back home.
The model was introduced last year in the Nicol Unit, in Stratford Hospital.
Although the trust reduced the number of beds, more patients have been treated through better use of beds, and enhanced and expanded services in the community.
Team members include rehabilitation assistants, nurses, occupational therapists and physiotherapists.
The team responds seven days a week from 8.30am until 10pm. At any one time, the team may be supporting 30 patients to stay at home by working with them daily.
They also offer rehabilitation to regain confidence and strength with daily living tasks that are necessary to remain living at home, for example, mobilising indoors, managing their stairs, maintaining personal care or preparing meals and drinks.
The team aims to reduce rising emergency admissions for people aged over 65 and reduce their hospital length of stay.
They also aim to integrate services across acute, community, GPs, social services and other organisations, for example Age UK.
The processes will ensure that only people who require hospital care will be in the hospital setting.
The day unit at Ellen Badger is also changing in line with the medical model and has been renamed to an Assessment and Rehabilitation Centre, refocusing care for patients and reflecting a new approach to rehabilitation.
“This will allow us, the local GPs and nurses, to treat more patients closer to home and the closer links with community services this will enable a quicker supported discharge home for inpatients.”
Source: stratford-herald.com
Hospitalized patients too often have no single physician in charge of their care
 Retired Alexandria internist Marsha Wallace had heard plenty of horror stories about hospital patients falling through the cracks. Still, she was troubled last fall during her own stay at a local hospital when she overheard doctors delivering entirely conflicting messages to the elderly cancer patient who was her roommate.
Retired Alexandria internist Marsha Wallace had heard plenty of horror stories about hospital patients falling through the cracks. Still, she was troubled last fall during her own stay at a local hospital when she overheard doctors delivering entirely conflicting messages to the elderly cancer patient who was her roommate.
“First the surgeon came in and told her he hadn’t found anything,” Wallace recalled. “Then the gastroenterologist came in and said, ‘I just did a CT scan; you have an obstructed kidney.’ Then the internist came in and said, ‘We don’t know what’s wrong, so we may send you to [Johns] Hopkins.’ Then the social worker came in and said, ‘We’re going to discharge you to a rehab hospital.’ ”
The caregivers didn’t appear to be talking to one another, Wallace said.
Coordinated care, touted as the key to better, more cost-effective care, is being encouraged through financial rewards and penalties under the 2010 health-care overhaul, as well as by private insurers. But experts say communication failures remain disturbingly common.
“Nobody is responsible for coordinating care,” said Lucian Leape, a Harvard health-policy analyst and a nationally recognized patient safety leader. “That’s the dirty little secret about health care.”
Advocates for hospital patients and their families say confusion about who is managing a patient’s care and the failure of caregivers to collaborate are endemic, contributing to an estimated 44,000 to 98,000 deaths from medical errors each year. A landmark report by the Institute of Medicine in 1999 cited the fragmented health-care system and patients’ reliance on multiple providers as a leading cause of medical mistakes. Leape, who helped author that report, says there have been improvements since, but “we have not done enough.”
Subsequent studies suggest the toll may be even higher than the Institute of Medicine estimated. A 2010 federal report projected that 15,000 Medicare patients every month suffered such serious harm in the hospital that it contributed to their deaths.
Betsy Gabay, 50, of Queens, barely survived her hospital stay last year for a flare-up of ulcerative colitis.
During her 26 days at New York Hospital Queens, she was seen by at least 14 different doctors, she said, and “I couldn’t tell one name from the next. I didn’t know whether it was the gastroenterologist or the nutritionist or the physical therapist.” All the time, she was rapidly deteriorating, suffering from acute abdominal pain and bloody diarrhea, and too weak to get out of bed. The medical staff decided to send her to a rehab hospital.
“I thought I was being sent there to die,” Gabay said.
That’s when her then 74-year-old mother took action. She contacted a physician friend who got Gabay admitted to Mount Sinai Medical Center in Manhattan. By then, Gabay had a blood clot in her lung and a serious bacterial infection. She also needed to have her diseased colon removed. After surgery and treatment at Mount Sinai and several months of recuperation at home, she has made a complete recovery.
Source: washingtonpost.com
BPJS Harus Menjamin Pasien Penyakit Berat
 Jakarta, PKMK. Badan Penyelenggara Jaminan Sosial Kesehatan (BPJS Kesehatan) harus menjamin biaya pengobatan pasien penyakit berat. Penyakit yang dimaksud antara lain bedah jantung, hemodialisis, lupus, dan lain-lain. Sebab, Undang-undang Nomor 40 Tahun 2004 tentang Sistem Jaminan Sosial Nasional (SJSN) dan Peraturan Presiden Nomor 12 Tahun 2013 menyebutkan tentang penjaminan tersebut. Hal ini disampaikan Rof. Hasbullah Thabrany, pakar Ilmu Kesehatan Masyarakat dari Universitas Indonesia di Jakarta (30/4/2013).
Jakarta, PKMK. Badan Penyelenggara Jaminan Sosial Kesehatan (BPJS Kesehatan) harus menjamin biaya pengobatan pasien penyakit berat. Penyakit yang dimaksud antara lain bedah jantung, hemodialisis, lupus, dan lain-lain. Sebab, Undang-undang Nomor 40 Tahun 2004 tentang Sistem Jaminan Sosial Nasional (SJSN) dan Peraturan Presiden Nomor 12 Tahun 2013 menyebutkan tentang penjaminan tersebut. Hal ini disampaikan Rof. Hasbullah Thabrany, pakar Ilmu Kesehatan Masyarakat dari Universitas Indonesia di Jakarta (30/4/2013).
Thabrany menambahkan, dalam UU SJSN jelas disebutkan bahwa pengobatan penyakit jantung dan hemodialisis dijamin oleh BPJS Kesehatan. Adapun penyakit lupus tidak disebutkan, namun harus dijamin. Transplantasi organ tubuh pun dijamin jika tersedia donor organ. “Jadi, semua penyakit harus dijamin,” kata Hasbullah. Definisinya, semua penyakit atas dasar indikasi medis dijamin oleh BPJS Kesehatan. Sejauh dokter mengatakan bahwa pasien akan meninggal kalau tidak diobati, BPJS Kesehatan harus menjamin pengobatannya, ungkap Hasbullah.
Lebih jauh ia berkata, tidak ada masalah bila 1,5 juta penderita lupus dijamin. Biaya besar bukan persoalan karena nantinya ada sekitar 230 juta jiwa yang akan membayar biaya kesehatan secara nasional. Melalui data tersebut, dapat ditafsirkan jumlah 1,5 juta penderita lupus tidak sampai 1 persen dari 230 juta jiwa. “Jika pengobatan penderita lupus ditanggung bersama, maka akan terasa ringan. Lain halnya bila mereka menanggung orang per orang,” jelas dia. Misalnya sampai kini penderita lupus belum mendapat kepastian, itu lebih karena masalah teknis. Peraturan Presiden Nomor 12 Tahun 2013 jelas menyebutkan bahwa semua penyakit atas indikasi medis dijamin pengobatannya, kata Hasbullah. Maka, sebagai penyelenggara BPJS Kesehatan, nantinya PT Askes harus menjamin pengobatan penderita lupus. “Tidak perlu ada kekhawatiran bahwa utilisasi sistem jaminan sosial nasional yang terlalu tinggi akan menjebol anggaran negara. Di dunia tidak ada bukti nyata atas hal tersebut. Sistem itu malah melahirkan efisiensi terhadap biaya belanja kesehatan nasional,” kata Hasbullah.