More than 25,000 people died of cancer in acute-care hospitals in 2011-12
About half of deaths among terminal cancer patients in Canada happen in hospitals, according to a new report.
The Canadian Institute for Health Information looked at end-of-life care for people with cancer across the country, excluding Quebec.
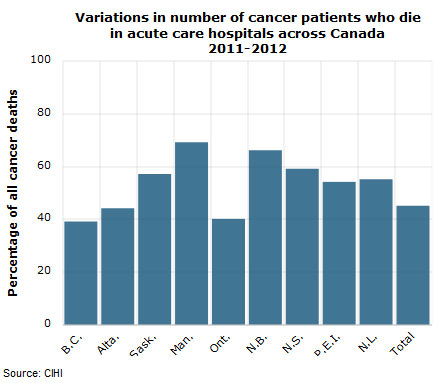
More than 25,000 people — or 45 per cent of all cancer deaths — died in acute-care hospitals in 2011-12, the institute said in its report Tuesday.
“What our study found was a bit of a mismatch between where patients said they wanted to die, which was at home, and where they did spend their last days,” said Kathleen Morris, the group’s director of health system analysis and emerging issues in Toronto.
“Many of the lesson learned from this study extend to anyone at end of life. People are looking for a well co-ordinated system, to have consistent caregivers, to have their pain managed and to be provided with the support they need.”
CIHI said the percentage of cancer patients who die in hospital ranges from 69 per cent in Manitoba to 39 per cent in British Columbia. Differences in the availability and location of palliative care beds in some provinces may be contributing to the variations between provinces in in-hospital beds, the group said.
In Winnipeg, end-of-life patients get dedicated doctors and case workers who oversee care outside of hospitals, said Dr. Michael Hosta of the Winnipeg Regional Health Authority.
“One of the unique aspects to our service is the ability to directly access palliative care beds, bypassing the emergency department,” Hosta said.
Strengthening services outside hospital
About 82 per cent of patients had a documented palliative care diagnosis during their last admission. It’s not known what specific palliative care services people received, or how many may have had access to it at hospices or through home care.
When Teresa Pilarski, 86, died of breast cancer at her daughter’s Toronto-area home on April 12, the family said they wanted to respect the frail woman’s wishes not to treat the cancer and to spend her final days as comfortable as possible in a familiar setting.
Daughter Dorothy Pilarski called the at-home palliative care from myriad professionals an “outstanding” complement to the support of family members and friends.
“She did express a tremendous amount of gratitude and a tremendous amount of affection, and that kept us going,” Dorothy Pilarski said, her voice breaking with emotion.
The experience was so rewarding that the family wants to encourage others to consider the option.
Pilarski’s physician, Dr. Harvey Pasternak, said the goal is to control symptoms with less anxiety to the patient and to their family.
CIHI also reported that 30 per cent of rural residents with cancer had multiple hospital admissions in their last four weeks of life, compared to 20 per cent of the urban residents.
Multiple hospital visits near the end of life can be difficult for individuals and their caregivers, when compared with care received at home, in a nursing home or a hospice, Morris acknowledged.
“Anything that can be done to improve the consistency of care and co-ordination would be very helpful,” she said.
Strengthening services outside the hospital system, such as through family doctors, hospice care or support in the home, are all possibilities, Morris said.
Source: http://www.cbc.ca